Ever gotten blood test results back and felt like your doctor was speaking a foreign language? You’re not alone. When my MCH came back “low,” my doctor said “take some iron pills” and moved on. But after months of iron supplements with zero improvement, I knew there had to be more to the story.
The normal range for MCH (mean corpuscular hemoglobin) is considered to be “27-33 picograms (pg)” according to Anadolu Medical Center, but what your doctor might not tell you is that these “abnormal” values often show off your body’s clever workarounds that have kept your ancestors alive for thousands of years. Most people think low MCH simply means iron deficiency, but what I’ve learned (and wish someone had told me sooner) is that these numbers actually show how smart your body is at managing its resources.
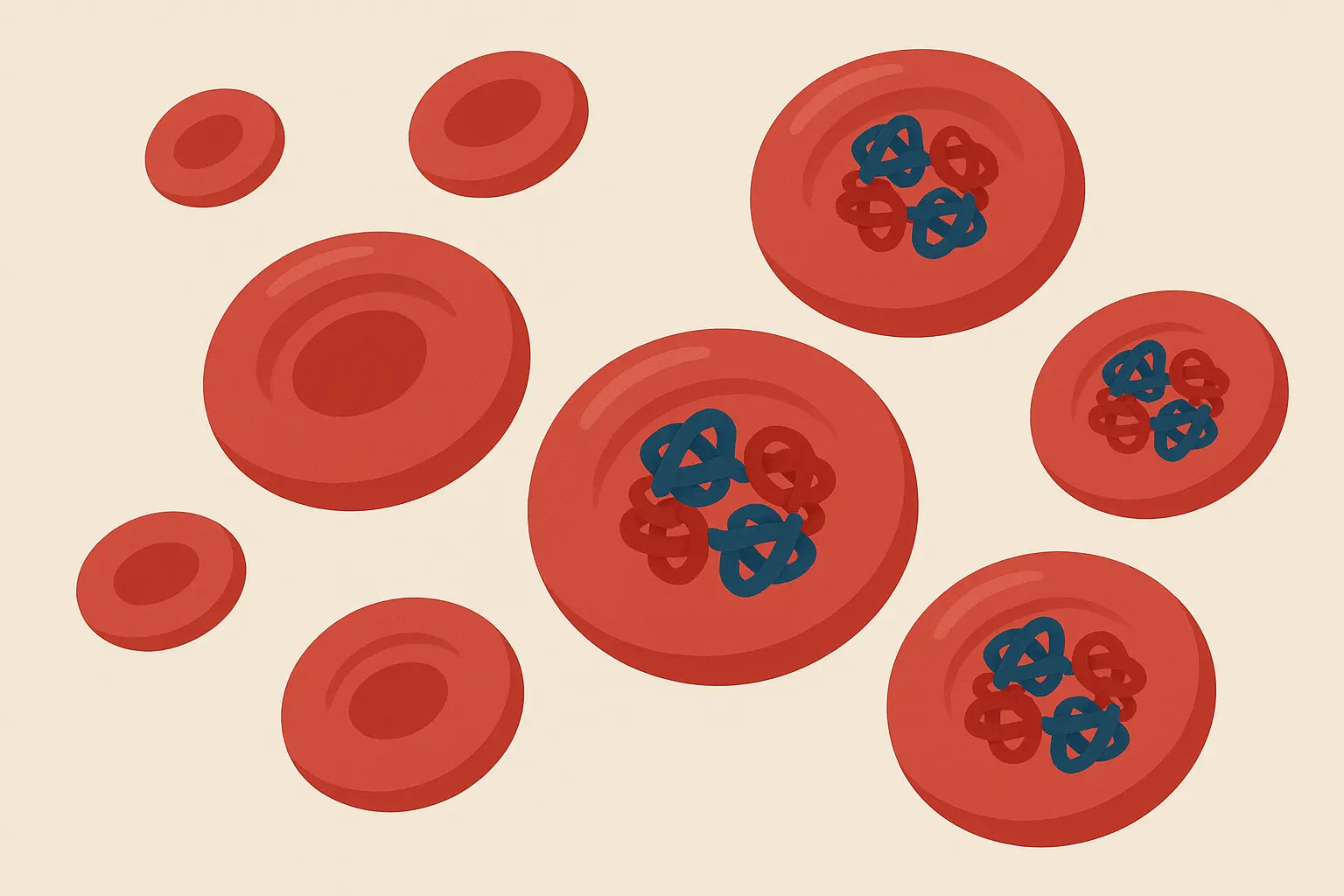
Table of Contents
- The Real Story Behind Your Body’s Oxygen Delivery System
- Going Beyond the “Just Take Iron” Advice
- Your Personal MCH Game Plan
- Tracking What Actually Matters
- The Bottom Line
TL;DR
- Low MCH shows how efficiently your body delivers oxygen at the cellular level, not just whether you need more iron
- Your body might be redirecting resources for immune function or healing instead of making more red blood cells
- The MCH-MCHC relationship tells you whether you have small, efficient cells or watered-down hemoglobin
- Some genetic traits make “abnormal” MCH values actually protective (thanks, ancestors!)
- Chronic inflammation messes with iron regulation through a hormone called hepcidin, blocking absorption even when you have plenty stored
- Nutrients like copper, B6, folate, and B12 work as a team – trying to fix just one usually doesn’t work
- Hidden blood loss from medications, exercise, or periods can outpace your replacement efforts
- Genetic testing reveals what types of iron work best for you and when to take them
- Iron absorption follows your body clock with peak efficiency in morning hours
- Getting the full picture requires more comprehensive testing than just basic ferritin
The Real Story Behind Your Body’s Oxygen Delivery System
Most people think low MCH simply means iron deficiency, but what I’ve discovered is that it’s actually a window into how your body makes really smart decisions about resources. Your cells are constantly figuring out where to invest precious materials, and low MCH often shows these complex choices rather than just nutritional problems. Understanding this perspective changes everything about how you approach getting better.
When I look at someone’s mch blood test low results, I’m seeing evidence of their body’s internal decision-making process. Your cells operate with remarkable intelligence, constantly evaluating where to invest precious resources based on what they need to survive right now. This affects how your body makes energy in ways that traditional medical thinking completely misses.
Your Body’s Hidden Resource Management System
Low MCH isn’t just about having smaller red blood cells – it’s your body’s way of managing a complex distribution network for iron and protein resources. When I see low MCH values, I’m looking at evidence of your body’s internal triage system, where resources get redirected based on what you need to survive right now.
Understanding how your body manages cellular resources becomes even more important when you explore the importance of genetics in personalized healthcare, as genetic variants significantly influence how efficiently your cells handle iron and hemoglobin production.
The Hemoglobin Distribution Game Your Body Plays
MCH measures the average amount of hemoglobin per red blood cell, but what’s really happening is your body making calculated decisions about where to invest iron and protein. Your body might be choosing to use these precious materials for other critical functions instead of making more red blood cells.
According to Medscape, “Adults/older adults/children: 32-36 g/dL (or 32-36%)” represents the normal MCHC range, but this standardized range doesn’t account for individual genetic variations that might make lower values actually protective. The relationship between MCH and MCHC becomes crucial here – when you understand how these markers work together, you can decode what your body is actually trying to tell you.
When Your Body Chooses Survival Over Oxygen Transport
Your body operates like a really smart CEO, and sometimes it prioritizes iron for other processes over making hemoglobin. This creates a cellular triage system where your energy levels get affected differently than the standard fatigue patterns doctors expect to see.
I’ve seen this countless times – people with low MCH who don’t fit the typical “tired and weak” profile because their bodies have found alternative ways to keep functioning. Your cells might be saying, “We need this iron for immune function right now, not for making more hemoglobin.”
Take my friend Sarah, a marathon runner whose MCH consistently tested at 24 pg (well below the normal 27-33 pg range). Despite her “abnormal” results, she maintained excellent endurance and energy levels. Further testing revealed she carried a minor thalassemia trait – her smaller, more efficient red blood cells were actually an evolutionary advantage that protected her ancestors from malaria while giving her enhanced oxygen use during long runs.
The Protein Strategy You Never Knew About
Low MCH often shows your body’s decision to use amino acids for immune function or healing rather than red blood cell production. This indicates underlying recovery demands that standard blood tests can’t capture.
Think about it – if you’re fighting off infections, healing from workouts, or dealing with stress, your body needs those amino acids for more immediate concerns than building red blood cells. The low MCH becomes a breadcrumb trail leading to these hidden recovery processes. Your MCHC levels help distinguish whether this is happening – when MCHC stays normal despite low MCH, you’re looking at smart resource management rather than true deficiency.
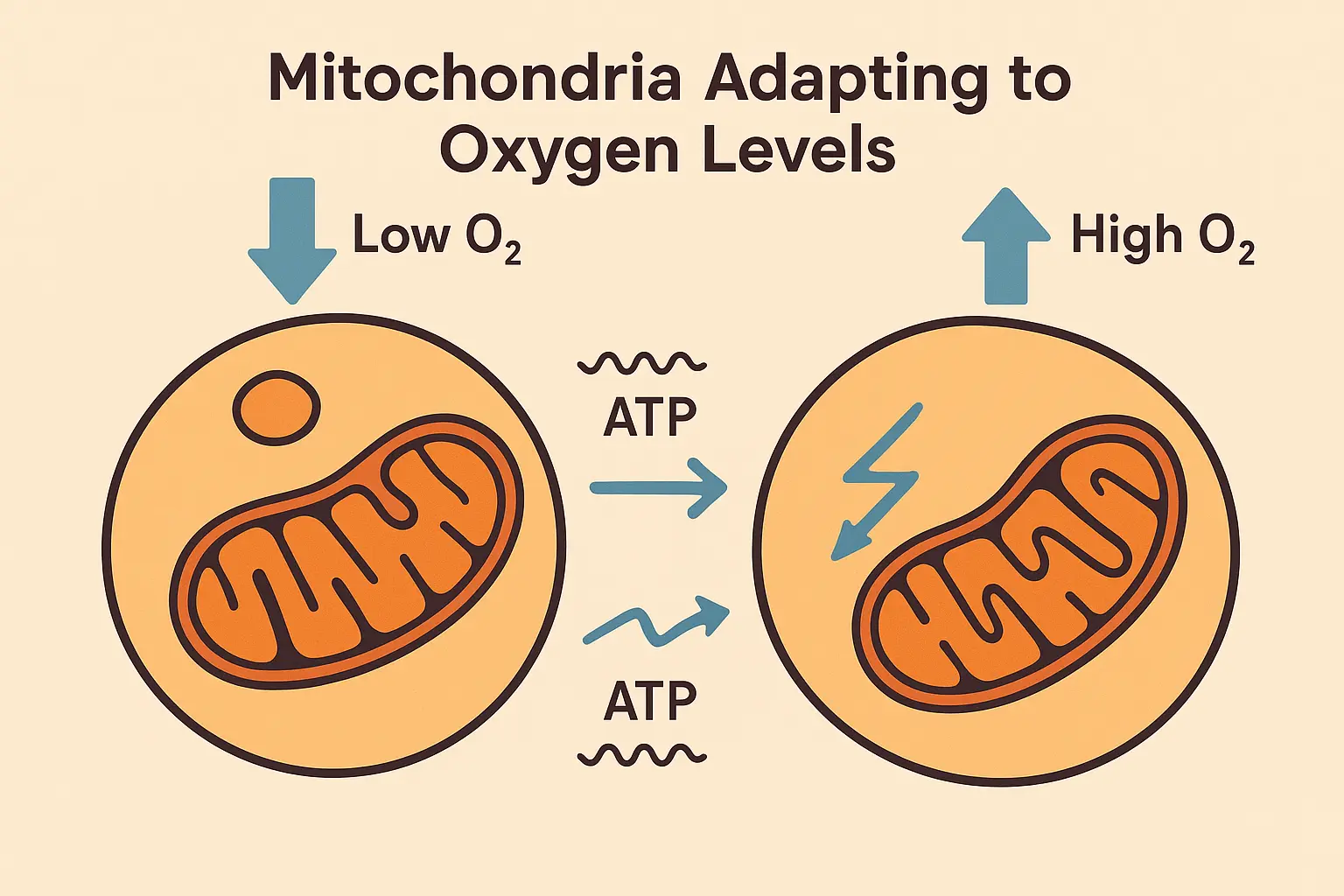
Your Mitochondria’s Clever Adaptation Trick
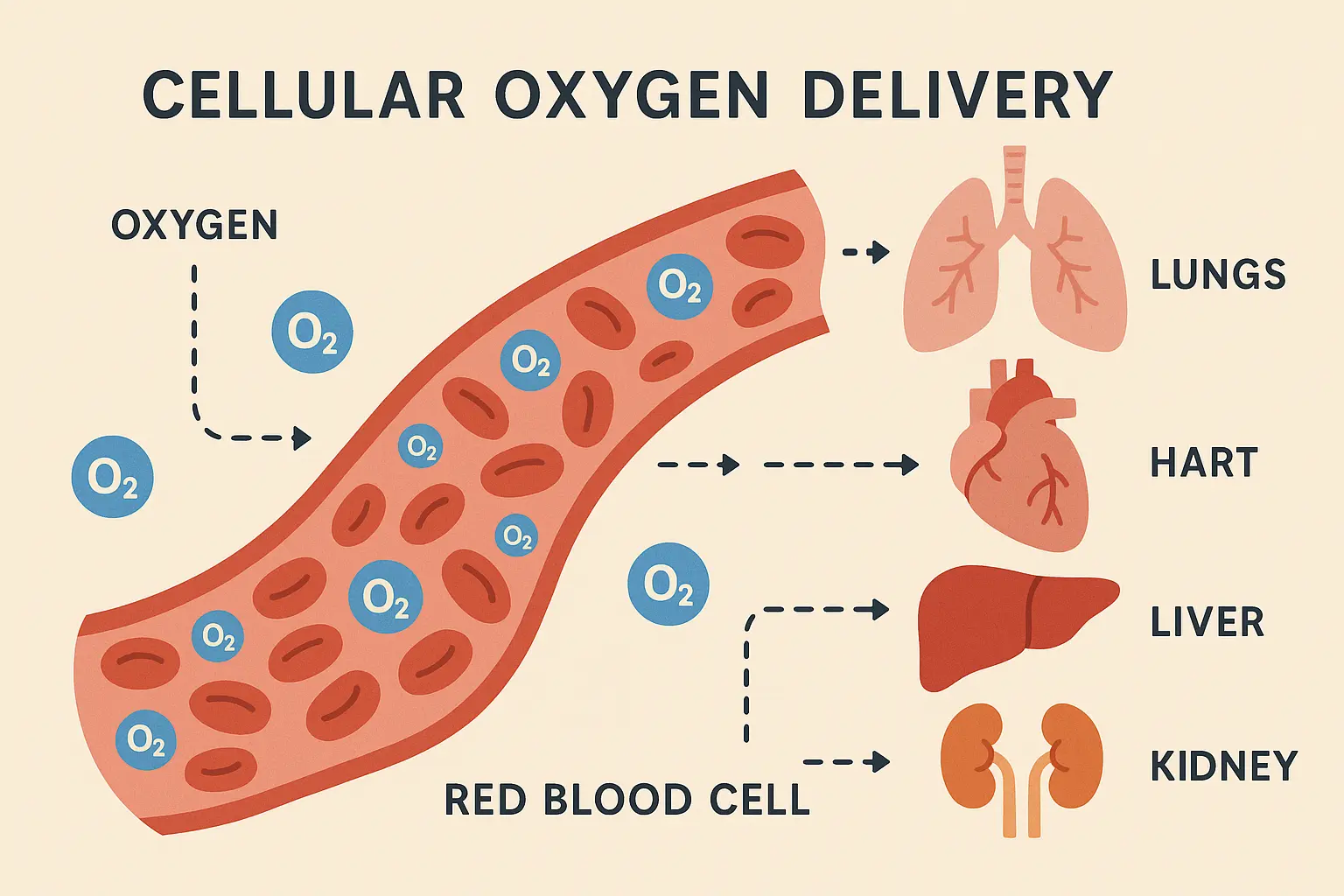
Your cells may be adapting to lower oxygen-carrying capacity by making their mitochondria more efficient, creating a backup plan that standard tests don’t capture. This cellular adaptation can actually improve how flexible your metabolism is in unexpected ways.
Your mitochondria are incredibly adaptable. When they sense reduced oxygen delivery, they don’t just sit there and complain – they get more efficient. This adaptation might explain why some people with consistently low MCH don’t experience the fatigue you’d expect. The MCHC values often provide clues about whether this adaptation is working successfully.
Decoding the MCH-MCHC Relationship
The relationship between MCH and MCHC (Mean Corpuscular Hemoglobin Concentration) reveals whether your red blood cells are small but efficient or if hemoglobin is watered down within normal-sized cells. This distinction completely changes your treatment approach.
This complex interplay between different blood markers highlights why improving blood test results requires a systematic approach that addresses underlying cellular function rather than just isolated nutrient deficiencies.
| MCH Status | MCHC Status | Cell Characteristics | Likely Causes | Treatment Approach |
|---|---|---|---|---|
| Low | Normal | Small, efficient cells | Genetic traits, thalassemia | Monitor, genetic testing |
| Low | Low | Watered-down hemoglobin | Iron deficiency, inflammation | Iron supplementation, investigate inflammation |
| Normal | Low | Normal size, poor concentration | Chronic disease, B12/folate deficiency | Address underlying condition |
| High | Normal | Large, normal concentration | B12/folate deficiency | Vitamin supplementation |
The Concentration vs. Content Mystery
When MCH is low but MCHC is normal, your cells are smaller but packed efficiently with hemoglobin. When both are low, you’re dealing with watered-down hemoglobin content that requires completely different interventions.
This distinction matters more than most doctors realize. Small, efficient cells might indicate genetic traits that are actually protective. Watered-down cells suggest active processes that need immediate attention. The MCHC measurement becomes your diagnostic compass here – it tells you whether you’re dealing with cellular efficiency or cellular dysfunction. Understanding these MCHC patterns helps you avoid unnecessary treatments and focus on what your body actually needs.
Your Genetic Blueprint for Blood Formation
Low MCH can indicate specific genetic variants affecting iron absorption, heme synthesis, or globin chain production. Understanding these variants influences your personalized treatment approach and helps explain why standard protocols might not work for you.
The Thalassemia Trait Advantage
Many people with consistently low MCH carry minor thalassemia traits that actually provide malaria resistance, making their “abnormal” values evolutionarily advantageous. This genetic variant explains why some people feel fine despite concerning lab values.
If you’ve got Mediterranean, African, or Southeast Asian ancestry, your low MCH might be a feature, not a bug. These genetic variants protected your ancestors from malaria, and they’re still protecting you in ways we’re just beginning to understand.
Your Personal Iron Absorption Fingerprint
Your DNA basically gave you an instruction manual for how your body handles iron. Some people got the “absorb everything” version, others got the “be super selective” version. Neither is wrong – they’re just different approaches that helped our ancestors survive different challenges. The MCHC values help track whether your personalized approach is working – when MCHC improves alongside MCH, you know you’ve found the right strategy for your genetic makeup.
Going Beyond the “Just Take Iron” Advice
Addressing low MCH requires detective work that goes way beyond simple iron deficiency. What I’ve learned is that inflammation, nutrient team problems, and hidden bleeding sources create complex patterns that conventional medicine often overlooks. This investigative approach reveals the real culprits behind persistent low MCH values.

The Root Cause Detective Work
Low MCH requires a forensic approach to health, examining inflammation, nutrient team deficiencies, and hidden bleeding sources that conventional medicine routinely misses. This detective work often reveals surprising connections between seemingly unrelated symptoms and your blood test results.
The complexity of nutrient interactions becomes particularly evident when examining B12 deficiency patterns, which can significantly impact red blood cell formation and contribute to persistently low MCH values despite adequate iron intake.
The Inflammation-Iron Connection Nobody Talks About
Chronic low-grade inflammation can shut down red blood cell production and iron use, creating low MCH that won’t respond to iron supplementation alone. This inflammatory suppression pathway explains why some people take iron supplements for months without improvement.
Here’s what’s really frustrating – you can take all the iron supplements in the world, but if inflammation is blocking utilization, you’re essentially pouring water into a bucket with holes in it. The MCHC levels often stay low alongside MCH when inflammation is the culprit, giving you a clear diagnostic pattern.
Hepcidin: The Iron Gatekeeper Gone Rogue
There’s this hormone called hepcidin that acts like a bouncer at your cells’ door. When you’re inflamed or fighting something off, it gets way too aggressive about blocking iron from getting in – even when you actually need it.
Hepcidin becomes the overly strict bouncer at the cellular level, and when inflammation cranks up, it blocks iron entry even when your storage levels look fine on paper. Your cells are literally starving for iron while your storage levels appear adequate.
Recent research highlighted by “Metropolis Healthcare” emphasizes that “MCHC measures the amount of haemoglobin in red blood cells. Combined with other CBC values, it is most helpful in determining the underlying causes of anaemia and predicting prognosis in those without anaemia,” indicating a shift toward more comprehensive blood analysis approaches. This MCHC blood test approach helps identify when inflammation is masking true iron status.
The Nutrient Team That Creates Perfect MCH
MCH production requires a team of nutrients working together – copper, B6, folate, and B12. Trying to fix just one nutrient misses these complex deficiency patterns where multiple players need to be in harmony for optimal red blood cell production.
The Copper-Iron Dance
Copper deficiency prevents iron utilization for hemoglobin synthesis, creating functional iron deficiency despite normal iron levels. This mineral interaction explains why iron supplementation alone often fails to improve MCH values.
Copper and iron work together as essential partners – when one is missing, the whole performance falls apart. I’ve seen people supplement iron for years without realizing their copper deficiency was the real problem.
The B-Complex Web of Dependencies
Folate and B12 deficiencies affect DNA synthesis in developing red blood cells, while B6 is essential for heme production. These interconnected deficiency webs create complex patterns that require comprehensive nutritional support.
Understanding these B-vitamin dependencies becomes crucial when considering folate metabolism variations, as genetic polymorphisms can significantly impact how efficiently your body utilizes these critical nutrients for red blood cell formation.
Research shows that “MCH values may be elevated due to larger, less efficient red blood cells” in conditions like leukemia, emphasizing how cellular size and efficiency work together to determine optimal oxygen delivery. The MCHC measurements help distinguish between these different cellular patterns and guide appropriate interventions.
The Hidden Blood Loss Investigation
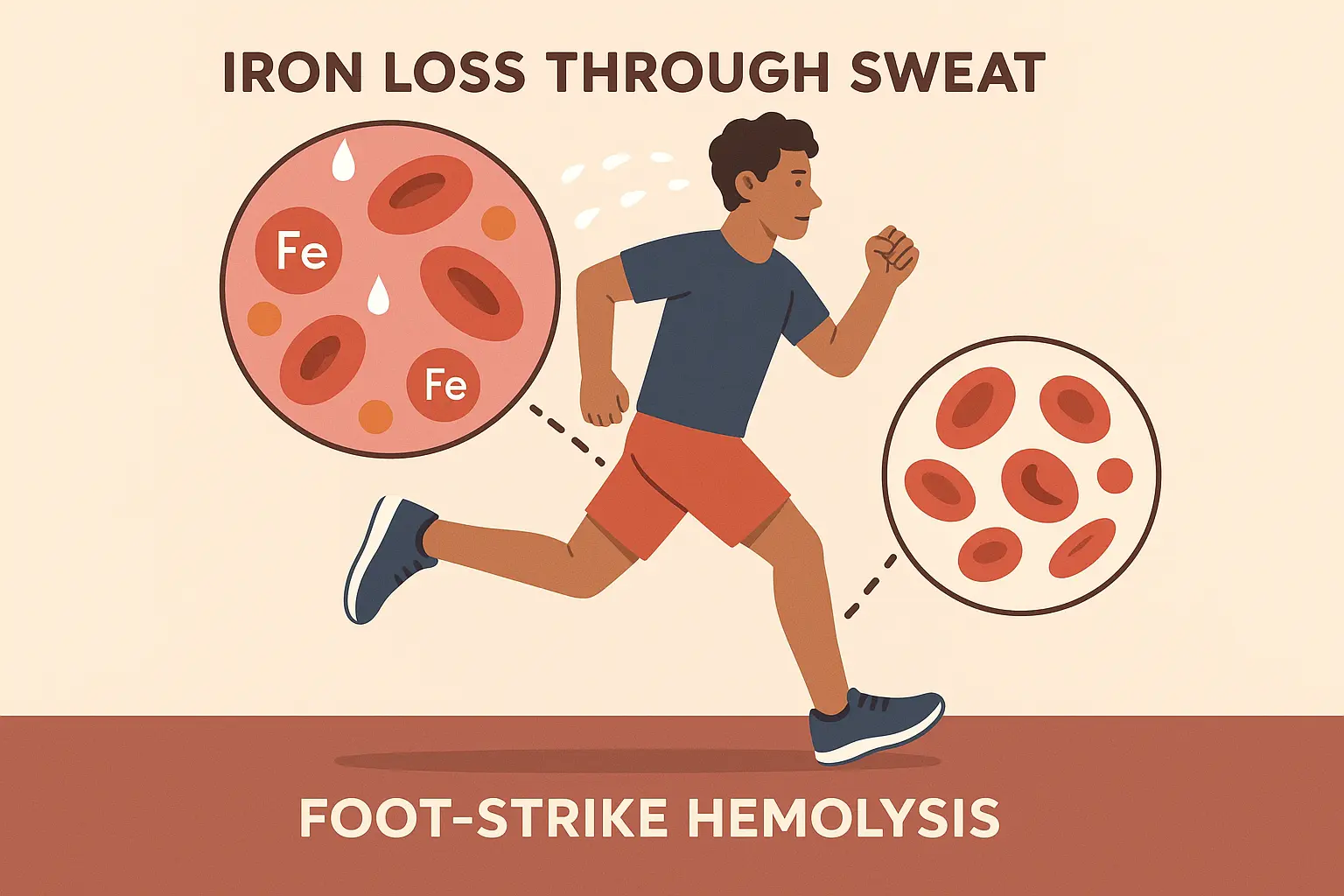
Tiny amounts of bleeding from sources like heavy periods, GI inflammation, or medication side effects can create ongoing iron loss that outpaces replacement efforts. Finding these hidden sources is crucial for successful MCH optimization.
The Period Math Most Women Don’t Know
Women lose 1mg of iron per day of menstruation, but heavy periods can create losses of 2-4mg daily. This requires precise calculation of replacement needs that goes far beyond standard recommendations.
Most women have no idea they’re losing this much iron. When you’re bleeding 2-4mg daily for 5-7 days every month, you need replacement strategies that account for this ongoing loss.
My friend Maria, a teacher, couldn’t understand why her MCH remained low at 25 pg despite taking iron supplements for six months. When we calculated her menstrual losses (heavy periods lasting 7 days = approximately 21-28mg iron loss monthly), it became clear her 18mg daily supplement wasn’t keeping pace with her 25mg average monthly losses, requiring both higher supplementation and investigation into her heavy bleeding.
Medications That Secretly Steal Your Iron
NSAIDs, aspirin, and certain supplements can cause tiny amounts of GI bleeding that slowly drain iron stores without obvious symptoms. This medication-induced microbleeding often goes undetected for years.
The Athlete’s Iron Paradox
Intense training can cause foot-strike hemolysis and increased iron losses through sweat, creating unique patterns in athletic populations. Exercise-induced hemolysis explains why some athletes struggle with persistently low MCH despite good nutrition.
Your Personal MCH Game Plan
Effective MCH optimization requires understanding your unique genetic makeup, lifestyle factors, and metabolic patterns to create targeted interventions. This personalized approach moves beyond one-size-fits-all protocols to address your body’s specific needs and genetic predispositions. The MCHC values serve as your progress indicator, showing whether your interventions are actually working at the cellular level.
Building Your Personal Treatment Plan
Your genetic variants determine what types of iron work best for you, how much you need, and what other nutrients you require for maximum absorption and use. This personalized approach explains why standard protocols work for some people but fail for others.
What Actually Helped Me (And Might Help You):
- Get the FULL iron panel, not just ferritin
- Stop taking iron with coffee (I learned this the hard way)
- Test inflammatory markers to see if that’s blocking things
- Check B-complex status, especially B12 and folate
- Look at copper and zinc levels
- Review medications for iron-stealing effects
- Calculate your actual iron replacement needs
- Get tested in the morning when your body absorbs iron best
- Consider genetic testing if nothing else works
- Track how you actually feel, not just numbers
Your Genetic Iron Protocol
Understanding your genetic variants helps determine the most effective iron forms, dosing strategies, and cofactor requirements for your unique physiology. This genetic-based approach maximizes absorption and utilization while minimizes side effects.
HFE Gene Variants and Your Iron Strategy
Common HFE variants affect iron absorption efficiency, requiring adjusted supplementation strategies and monitoring protocols. These genetic differences explain why some people need higher doses while others risk iron overload.
If you’ve got HFE variants, your iron absorption might be either supercharged or severely limited. Knowing this changes everything about your supplementation strategy.
The TMPRSS6 Gene’s Role in Iron Regulation
This gene affects hepcidin regulation, influencing how your body responds to iron supplementation and dietary iron sources. TMPRSS6 polymorphisms can make you either a super-absorber or someone who struggles with iron utilization. The MCHC patterns help reveal which category you fall into – consistent improvement suggests good absorption, while stagnant levels indicate genetic barriers.
Timing Your Iron for Maximum Absorption
Iron absorption follows your body’s daily rhythm, with peak absorption occurring in morning hours and reduced efficiency in evening. This timing strategy can significantly improve your supplementation results.
According to “UF Health”, CBC testing now includes “Mean hemoglobin amount per red blood cell (MCH)” as a standard parameter, reflecting the growing recognition of MCH’s importance in comprehensive health assessment beyond simple anemia screening.
The Morning Absorption Window
Taking iron supplements between meals on an empty stomach maximizes absorption, but requires careful timing to avoid stomach upset. The morning window offers the best compromise between absorption and tolerability.
Exercise Timing and Iron Interactions
Post-exercise iron supplementation can be less effective due to hepcidin elevation from exercise-induced inflammation. Understanding these timing interactions helps optimize your supplementation schedule.
The Enhancement and Inhibition Game
Combining iron with specific enhancers while avoiding inhibitors creates optimal absorption conditions and faster MCH improvement. This strategic approach can triple your absorption rates.
| Enhancement Strategy | Absorption Impact | Timing | Inhibitors to Avoid |
|---|---|---|---|
| Vitamin C (100-200mg) | 3x increase | With iron supplement | Coffee, tea (2+ hours apart) |
| Heme iron sources | 15-35% absorption | Any time | Calcium supplements |
| Empty stomach | 2-3x increase | Morning fasting | Dairy products |
| Acidic environment | 50% improvement | With citrus/vinegar | Antacids, PPIs |
| Copper cofactor | Prevents deficiency | Daily maintenance | Zinc (taken separately) |
Vitamin C: Your Iron’s Best Friend
Taking 100-200mg vitamin C with iron supplements can triple absorption rates, but timing and form matter significantly. This enhancement strategy is one of the most effective ways to boost iron utilization. Watch your MCHC levels improve alongside MCH when you get this combination right.
The Polyphenol Problem
Coffee, tea, and certain foods can reduce iron absorption by up to 90%, requiring strategic spacing of consumption. Understanding these inhibitors prevents you from sabotaging your own efforts.
My friend David, an executive, was frustrated that his MCH remained at 26 pg despite taking iron supplements religiously. The breakthrough came when we discovered he was drinking coffee with his iron supplement every morning. By switching to taking iron with orange juice (vitamin C enhancer) and delaying coffee by 2 hours, his MCH improved to 29 pg within 8 weeks. His MCHC values showed similar improvement, confirming the cellular changes were real.
Tracking What Actually Matters
Optimizing MCH requires sophisticated tracking beyond basic blood tests, incorporating functional markers, symptom patterns, and performance metrics to guide treatment adjustments. This comprehensive monitoring approach ensures you’re making real progress, not just improving numbers on paper.

The Functional Iron Assessment Matrix
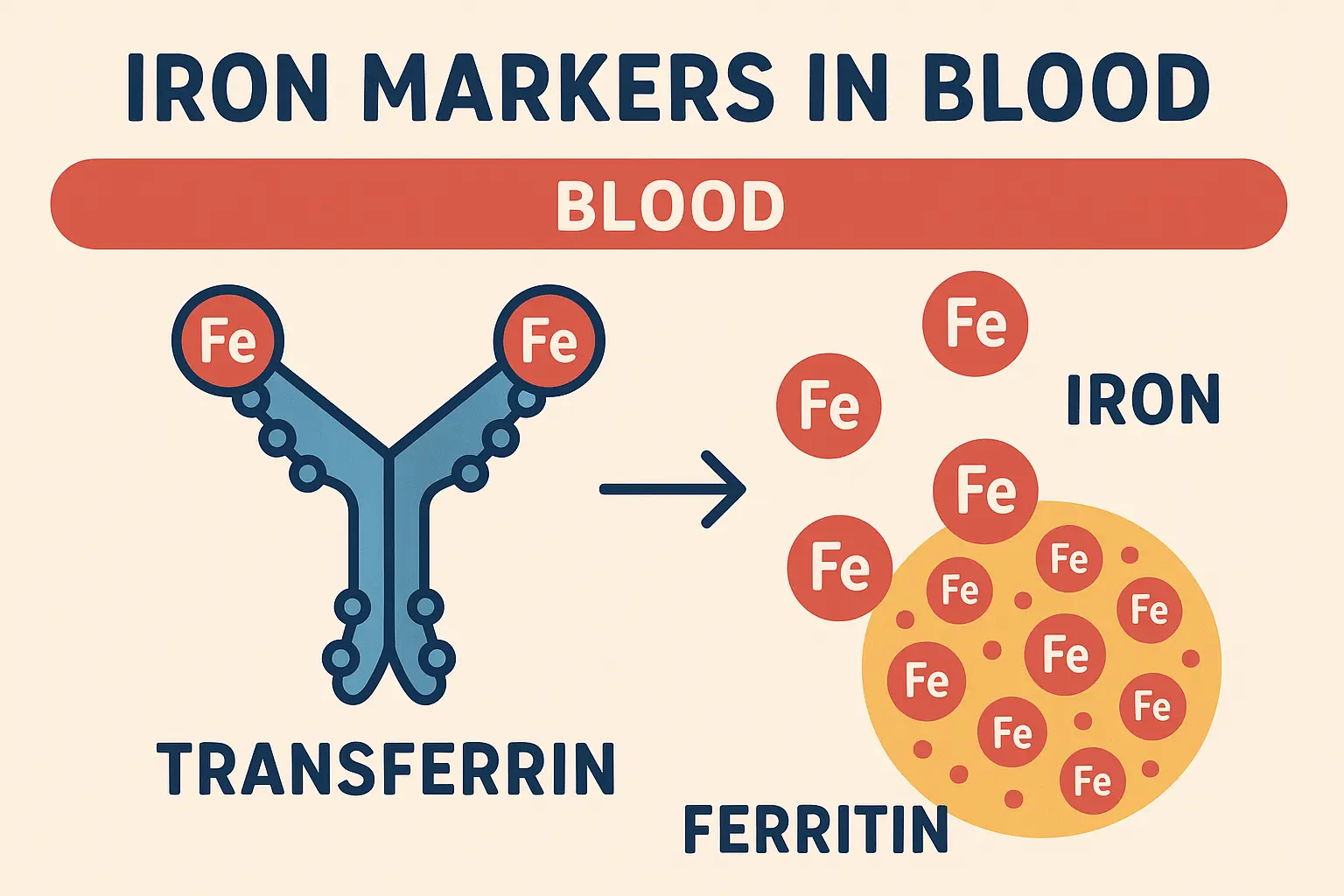
Standard iron tests miss functional deficiency patterns, requiring comprehensive panels that include ferritin, transferrin saturation, soluble transferrin receptor, and reticulocyte hemoglobin content. This matrix approach reveals the complete picture of your iron status.
According to “Health Shots”, “The normal reference ranges of this parameter are based on the demographics of the population. It is normally 27 to 33pg,” but demographic variations mean your optimal range might differ based on genetic ancestry and individual physiology. The MCHC measurements provide additional context for interpreting these ranges.
Reading Between the Ferritin Lines
Ferritin levels can be artificially elevated by inflammation, requiring hs-CRP correlation to distinguish true iron stores from inflammatory masking. This nuanced interpretation prevents misdiagnosis of iron status.
The Transferrin Saturation Story
This ratio reveals iron transport efficiency and helps distinguish between iron deficiency, inflammation, and genetic iron disorders. Transferrin saturation patterns provide crucial diagnostic information that ferritin alone can’t offer.
Performance-Based Outcome Tracking
MCH optimization should correlate with improved exercise capacity, cognitive function, and energy levels, providing functional validation of treatment effectiveness. These performance markers often improve before blood tests show changes.
Tracking these functional improvements aligns with strategies to improve blood oxygen levels, as enhanced MCH directly impacts your body’s oxygen-carrying capacity and cellular energy production.
How I Actually Track What’s Working (Without Becoming Obsessed):
Week 1-4 Baseline:
- How do I feel when I wake up? (Rate 1-10): ____
- Can I get through my afternoon without wanting to nap?: ____
- Do my hands and feet feel like ice cubes all the time?: ____
- Am I actually getting better at my workouts, or just going through the motions?: ____
- Brain fog episodes per day: ____
- Sleep quality (1-10): ____
Monthly Reality Check:
- MCH value: ____
- Ferritin level: ____
- Transferrin saturation: ____
- hs-CRP: ____
- How much better do I actually feel (%): ____
- Exercise capacity change (%): ____
Your VO2 Max Connection
Improved MCH should translate to better oxygen delivery and measurable improvements in cardiovascular performance metrics. Tracking VO2 max provides objective evidence of your optimization progress. The MCHC improvements often correlate with these performance gains.
The Brain Fog Barometer
Brain fog, concentration difficulties, and memory issues often improve as MCH normalizes, providing subjective validation of treatment success. These cognitive improvements frequently occur before blood markers fully normalize.
For those looking to take a comprehensive approach to optimizing their MCH and overall cellular health, Enov.One offers personalized functional health solutions that align perfectly with this nuanced understanding. Their platform integrates wearables data with detailed health assessments to create the complete metabolic picture needed for addressing complex issues like low MCH. With monthly adjustments to medication plans and smart supplementation based on your evolving data, you can move beyond simple iron supplementation to a truly personalized optimization strategy.
The Bottom Line
Understanding your low MCH results through this cellular efficiency lens changes everything about your approach to treatment. Instead of just throwing iron supplements at the problem, you’re now equipped to investigate the real underlying causes – whether that’s genetic variants, inflammatory processes, hidden blood loss, or complex nutrient interactions.
The lightbulb moment for me was realizing my body wasn’t broken – it was just prioritizing differently. Your body is incredibly smart about resource management. When MCH is low, it’s often telling a story about competing priorities, adaptive mechanisms, and genetic advantages that standard medical interpretation completely misses. Your “abnormal” values might actually represent sophisticated biological strategies that have kept your ancestors alive for thousands of years.
Moving forward, remember that optimization is a process, not a destination. Your MCH values will fluctuate based on stress, inflammation, nutrient status, and genetic expression patterns. The goal isn’t to achieve some arbitrary “normal” range, but to understand what optimal looks like for your unique physiology and life circumstances. The MCHC values provide additional insight into whether your optimization efforts are creating real cellular improvements or just temporary numerical changes.
Look, I’m not a doctor, and I can’t tell you what’s right for your specific situation. But what I can tell you is that your body is way smarter than most people give it credit for. Those “abnormal” numbers might be telling a story worth listening to, not just a problem to fix with the first supplement you find on Amazon.
Take your time. Ask better questions. And remember – you know your body better than anyone else, even if the medical system sometimes makes you feel like you don’t.
