Last summer, I thought I was coming down with the flu. I felt feverish, exhausted, and generally awful. But when I checked my temperature, it was completely normal. Turns out, I was just really dehydrated from a long day working outside in the heat. That’s when I learned something pretty eye-opening about how our bodies work.
With an estimated 75% of adults not drinking enough water daily, dehydration has become this sneaky problem that goes way beyond just feeling thirsty. Here’s something most people don’t realize: when you’re really dehydrated, you can actually start feeling feverish—even when there’s nothing wrong with you.
I’ve been digging into this connection for years, and honestly, it’s way more interesting than I thought it would be. Your body has this whole temperature control system, and when dehydration messes with even one part of it, you can end up feeling genuinely sick without any actual illness.
What We’ll Cover
- Why Your Cells Start Overheating When You’re Dehydrated
- How Your Body Tricks Itself Into Thinking It’s Sick
- Why You Might Feel Feverish When Your Temperature Is Normal
- What Actually Works to Feel Better Fast
The Quick Version
When you’re dehydrated, your cells basically overheat because they’re working harder than they should. Your body gets confused and starts acting like it’s fighting off an infection—releasing all the same chemicals that cause real fevers.
Sometimes your brain misreads the signals and makes you feel feverish even when your temperature is totally normal. To fix it, you need more than just water—you need the right balance of electrolytes, and there’s actually a specific way to do it that works better.
The key is catching it early. By the time you feel thirsty, your body’s already been struggling for hours.
Why Your Cells Start Overheating When You’re Dehydrated
Most people think dehydration just makes you thirsty and tired. But here’s what I found out: when your cells lose water, they trigger this whole cascade of problems with your body’s temperature control.
Think of it like this—your cells are like tiny engines, and they need water to stay cool. When they don’t get enough, they start overheating, your blood can’t move heat around properly, and your kidneys go into overdrive. It’s like a perfect storm that makes you feel genuinely feverish. The symptoms of dehydration extend far beyond what we typically recognize, affecting temperature regulation in ways that can leave you feeling genuinely ill.
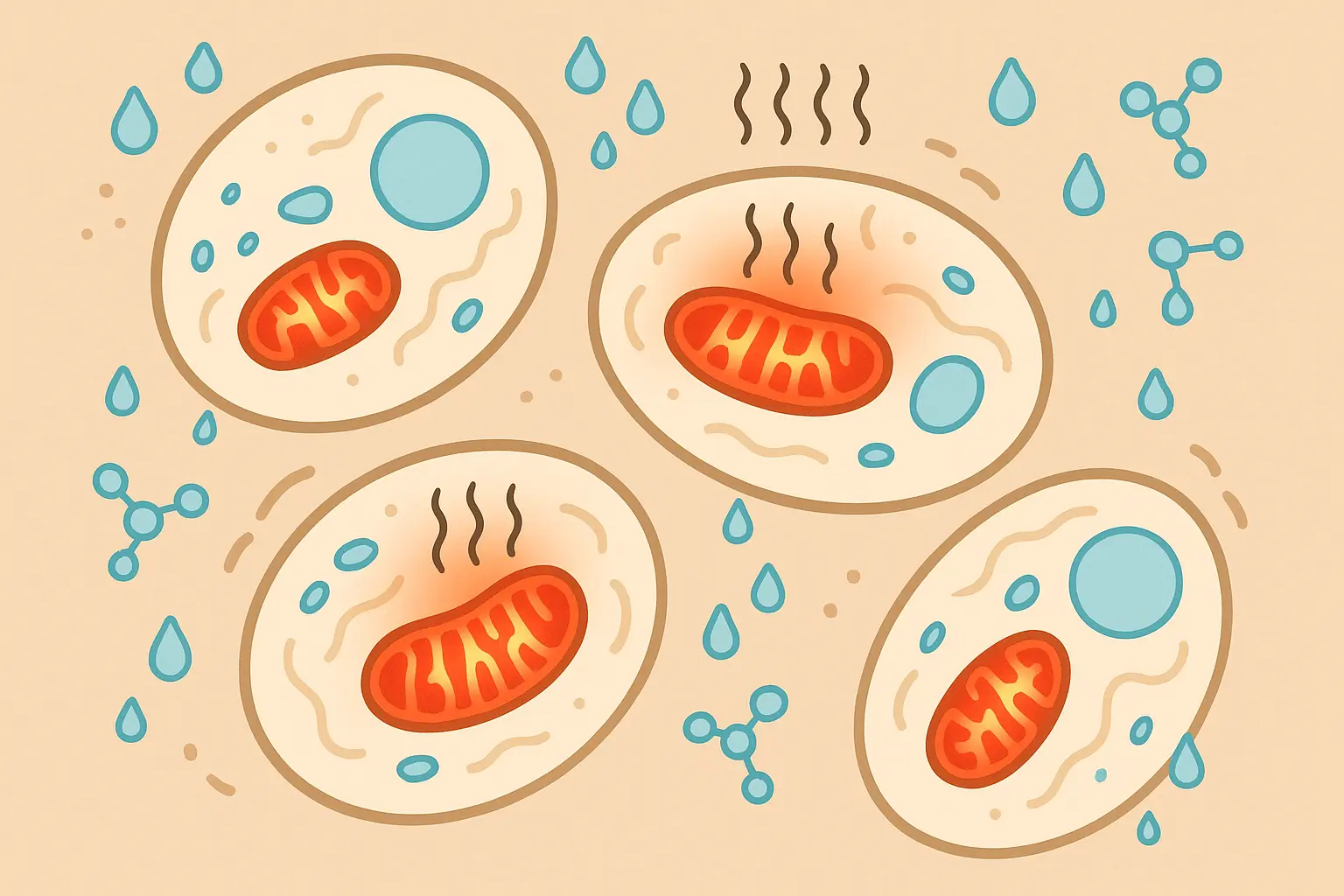
Your Body’s Energy Factories Are Working Overtime
Here’s what’s actually happening inside your cells when you’re dehydrated. Those little powerhouses called mitochondria start producing way more heat than normal. They’re basically working twice as hard to make energy without enough water, and all that extra effort creates heat.
It’s kind of like running your car engine without enough coolant—everything gets hot fast.
When dehydration sets in, your cellular engines run hot because they can’t get the cooling they need. This process creates a cascade of temperature-related problems that most people never connect to their hydration status.
Understanding how cellular energy production affects your overall health is crucial, and optimizing mitochondrial function becomes even more critical when dealing with dehydration-related temperature issues.
When Making Energy Becomes a Problem
Dehydrated cells can’t make energy efficiently anymore. Your cellular engines have to work overtime to produce the same amount of power, and all that extra work generates heat your body has to deal with.
I remember talking to Sarah, a marketing exec who thought she was getting sick during a crazy work week. She’d been drinking coffee all day but barely any water. By Thursday afternoon, she felt feverish and exhausted—no other symptoms, just felt awful. Her temperature was only 99.2°F, but she felt terrible.
After spending the evening rehydrating with some electrolyte drinks, she felt completely normal by the next morning. Her dehydrated cells had been working so hard to produce energy that they were literally generating excess heat. Once she got properly hydrated, everything went back to normal.
Your Proteins Start Freaking Out
Without enough water in your cells, your proteins start to clump together and misfold. Your body sees this as an emergency and cranks up your temperature to try and fix the protein damage—it’s like your body’s version of turning up the heat to melt ice.
This creates this weird feedback loop where your temperature goes up to protect your cells, but the higher temperature can actually stress your cells more. Your body is trying to solve one problem but accidentally creating another.
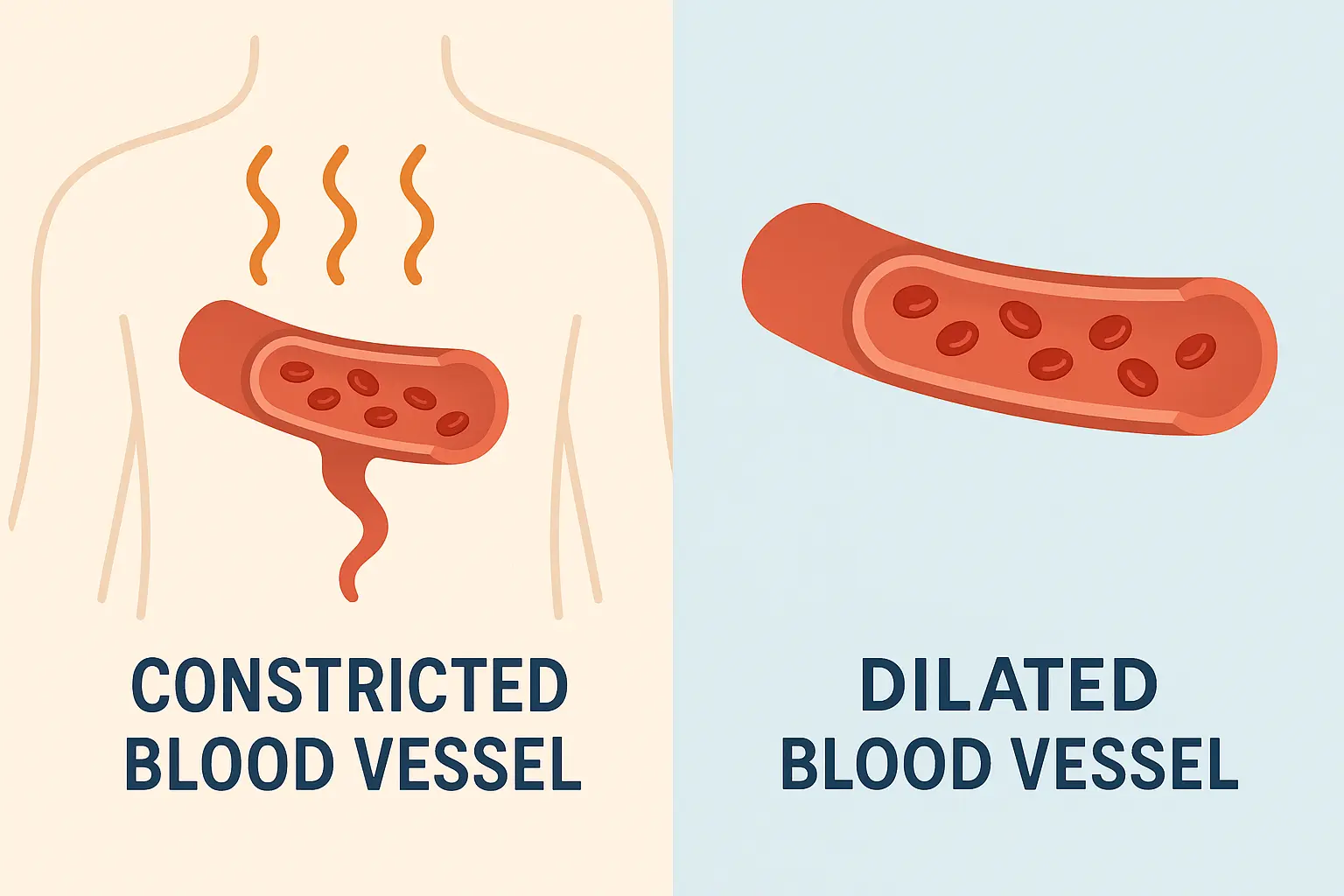
Your Cooling System Stops Working
Dehydration completely messes with your blood vessels’ ability to regulate heat. When your blood volume drops, your main cooling systems—sweating and getting blood to your skin—basically stop working right. Heat gets trapped, and your temperature climbs.
Think of your blood vessels like a car’s cooling system. When you don’t have enough coolant (blood), the radiator (your skin) can’t do its job of releasing heat.
Poor circulation from dehydration affects more than just temperature regulation, as detailed in our guide on improving blood circulation through energy systems, which becomes essential for recovery. When your circulation is compromised, every system in your body feels the impact.
| Hydration Level | Blood Volume Impact | Temperature Regulation Ability | Risk of Fever-Like Symptoms |
|---|---|---|---|
| Well Hydrated | 100% normal volume | Excellent vasodilation & sweating | Minimal risk |
| Mild Dehydration (2-5% fluid loss) | 95% normal volume | Reduced sweating efficiency | Low to moderate risk |
| Moderate Dehydration (5-10% fluid loss) | 85% normal volume | Impaired vasodilation | High risk |
| Severe Dehydration (>10% fluid loss) | <80% normal volume | Severely compromised cooling | Very high risk |
Not Enough Blood to Go Around
When you’re dehydrated, you literally have less blood volume. Your blood vessels can’t expand properly to bring warm blood to your skin surface where heat can escape. You also can’t sweat effectively, so heat just builds up in your system.
When you’re properly hydrated, your blood vessels can dilate to bring warm blood closer to your skin, letting heat escape. Without enough fluid, this whole system breaks down. Dehydration symptoms include this inability to regulate temperature effectively, leaving you feeling overheated even in normal conditions.
Your Brain’s Thermostat Gets Confused
Dehydration throws off your sodium and potassium levels, which directly messes with how your brain’s thermostat works. This can trigger false fever responses even when nothing’s actually wrong.
Your brain’s temperature control center needs precise electrolyte levels to function properly. When dehydration disrupts these levels, your brain starts making temperature decisions based on bad information. Staying hydrated maintains the delicate balance your brain needs to keep your temperature stable.
You might feel feverish when your temperature is normal, or struggle to cool down when you should. This dehydration-induced confusion in your brain’s thermostat can stick around even after you start drinking water again.
Your Kidneys Are Working Too Hard
When your kidneys have to work overtime to save water by concentrating your urine, they generate extra heat. It’s like your kidneys are literally heating you up while trying to conserve every drop of water they can.
This puts additional strain on organs that are already working harder because of dehydration. The heat your kidneys generate adds to the overall temperature your body has to manage.
How Your Body Tricks Itself Into Thinking It’s Sick
Here’s where it gets really interesting. Dehydration doesn’t just affect your temperature directly—it actually fools your immune system into thinking you’re under attack. Your body starts releasing the same inflammatory chemicals it would use to fight off an infection, creating real fever symptoms without any actual illness.
Recent medical research highlighted by “UNICEF Vietnam” shows that severe dehydration from conditions such as rotavirus-induced diarrhea can lead to life-threatening complications, with fever, vomiting, and diarrhea all contributing to dangerous fluid loss that creates a cascade of immune system responses.
I’ve seen this happen to people who deal with chronic dehydration. Their bodies essentially sound false alarms, triggering inflammatory responses that create genuine symptoms of dehydration including elevated temperature, fatigue, and feeling generally crappy.
Your Stress Hormones Go Into Overdrive
When you lose water, your body releases a flood of stress hormones like cortisol and adrenaline. These hormones can seriously elevate your body temperature by increasing your metabolic rate and messing with your circulation.
When dehydration stress hits, your adrenal glands respond like you’re facing a real threat. This hormonal flood affects multiple systems at once, creating problems that go way beyond simple fluid loss.
The hormonal cascade triggered by dehydration is complex, and understanding how to address hormonal imbalances naturally becomes crucial for long-term temperature regulation recovery. These imbalances can persist even after rehydration begins, requiring targeted intervention to fully resolve.
The Stress Spiral That Feeds Itself
High cortisol from dehydration stress increases protein breakdown and glucose production—both processes that generate significant heat. This creates this vicious cycle where stress from dehydration creates more heat, which creates more stress, which creates even more heat.
I heard about Michael, a construction worker who developed what looked like heat exhaustion during a summer job. His temperature hit 101.8°F, but blood tests showed no infection. Turns out severe dehydration had triggered such a massive cortisol spike that his metabolic heat production increased by almost 30%.
Once he got properly rehydrated with IV fluids, his cortisol levels dropped and his temperature went back to 98.4°F within four hours. The dehydration had created such an intense stress response that his body was essentially overheating itself from the inside out.
Your Body Releases Infection-Fighting Chemicals (But There’s No Infection)
Dehydration triggers the release of inflammatory molecules like interleukin-1 and tumor necrosis factor—the exact same chemicals your body uses to fight real infections. These molecules directly target your brain’s temperature centers, producing legitimate fever symptoms.
Your immune system sees severe dehydration as a serious threat and responds accordingly. The inflammatory chemicals released are identical to what happens during actual infections, which explains why dehydration-induced fever feels so real.
Your Brain’s Thermostat Gets Reprogrammed
Those inflammatory chemicals stimulate something called prostaglandin E2, which literally resets your brain’s thermostat to a higher temperature. You’re not imagining the fever—your brain has actually been reprogrammed to run hotter.
This reprogramming can take hours to reverse, even after you start rehydrating properly. The dehydration essentially hijacks your brain’s temperature control, forcing it to maintain higher temperatures until the inflammatory response calms down.
Full Immune System Alert
Severe dehydration can activate proteins that create an inflammatory state virtually identical to a bacterial infection. Your body genuinely believes it’s fighting off invaders and responds with all the fever-inducing mechanisms it would use against real threats.
This explains why people with severe dehydration often feel genuinely sick, not just thirsty or tired. Their bodies are mounting a full inflammatory response to what they perceive as a serious survival threat.
Why You Feel Feverish Without Actually Having One
Sometimes dehydration creates the weirdest symptom of all—feeling feverish when your actual temperature is completely normal. This happens because dehydration messes with how your nervous system processes temperature signals, creating fever experiences that feel totally real but don’t show up on a thermometer.
Medical experts from “Prevention Magazine” explain that experiencing chills without fever can indicate dehydration among other conditions, noting that “if you think you are experiencing chills due to dehydration, make sure to drink plenty of water and electrolytes.”
This neurological confusion is one of the most frustrating aspects of dehydration-related temperature problems. You feel genuinely feverish, but thermometer readings are normal, so many people dismiss their symptoms or think they’re imagining things. The symptoms of dehydration can include these phantom fever sensations that feel completely real to the person experiencing them.
I’ve run into this phenomenon repeatedly, and it’s often a sign that dehydration is affecting brain chemistry and nervous system function rather than actual temperature.
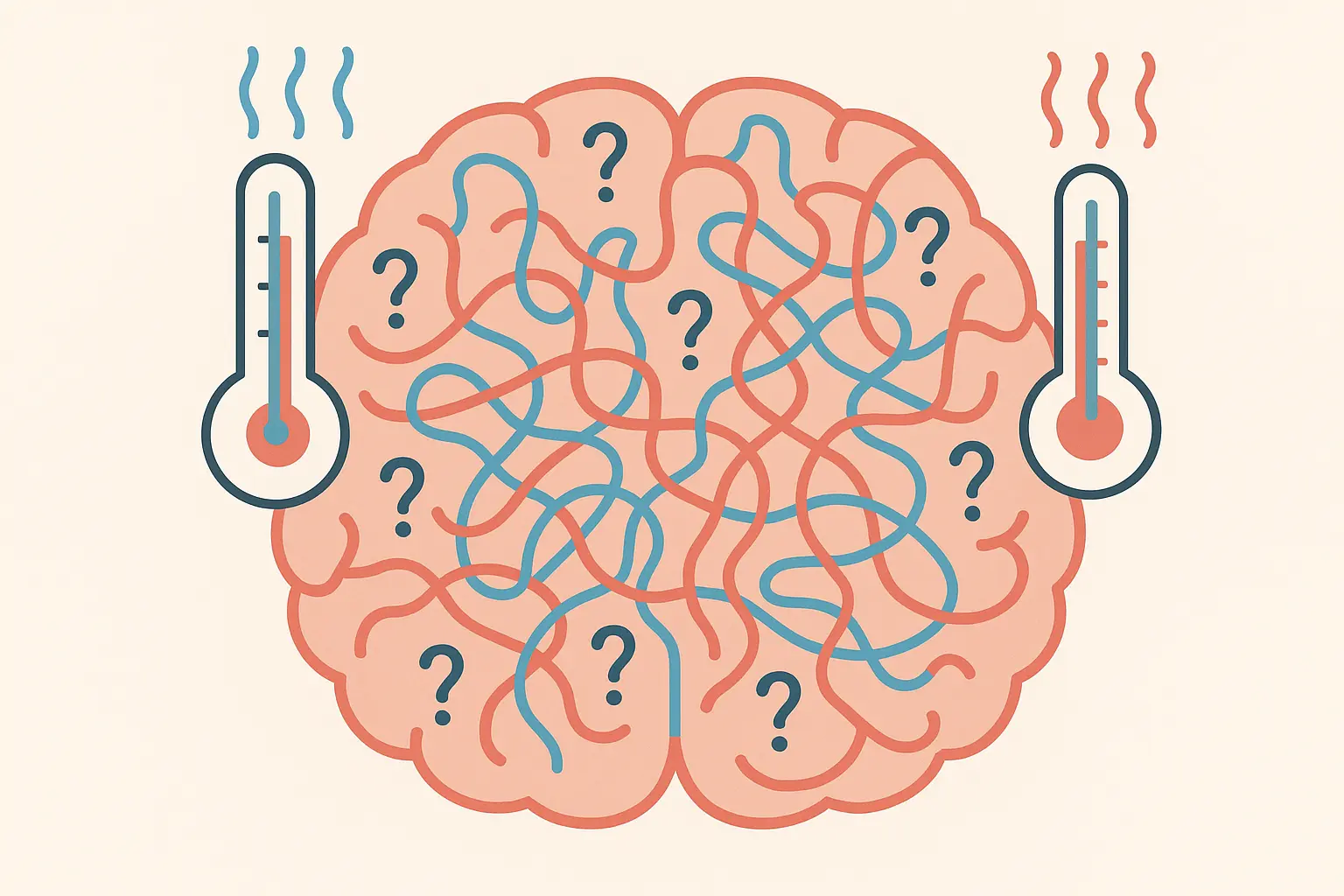
Your Brain Fog Affects Temperature Signals
Dehydration-induced brain fog doesn’t just make you feel mentally fuzzy—it actually affects your brain’s ability to accurately process temperature sensations. You might feel burning hot or shivery cold when your body temperature is perfectly normal.
When your brain doesn’t have adequate hydration to function optimally, sensory processing becomes unreliable. Temperature perception requires complex neural networks that depend on proper hydration to work right.
This cognitive disruption can make you feel like you have a fever when you don’t, or prevent you from recognizing when your temperature actually is elevated. Staying hydrated maintains the neural clarity needed for accurate temperature perception.
Your Brain Chemistry Gets Thrown Off
Water loss disrupts serotonin and dopamine production, and these brain chemicals play crucial roles in temperature perception. When they’re out of whack, you can experience false fever sensations that feel completely real.
Jennifer, a teacher, had recurring “fever episodes” every afternoon for two weeks. Her temperature was consistently normal at 98.6°F, but she felt feverish, had chills, and experienced brain fog. Her doctor figured out she was chronically dehydrated from drinking only coffee and diet soda all day.
After implementing a proper hydration routine with electrolyte supplements, her false fever sensations completely disappeared within five days. The dehydration had messed with her brain chemistry so much that her temperature perception was completely unreliable. Once properly hydrated, everything went back to normal.
The connection between hydration and cognitive function is profound, and our research on improving attention span through science reveals how proper hydration supports optimal brain chemistry. When your brain chemistry is balanced, temperature perception becomes accurate again.
Your Vagus Nerve Stops Communicating Properly
Dehydration affects your vagus nerve, which is like the main communication highway between your body’s temperature sensors and your brain’s processing centers. When this communication breaks down, you can get completely inappropriate temperature sensations.
Your vagus nerve carries critical information about your body’s internal state to your brain. When dehydration impairs this nerve’s function, your brain receives garbled or incomplete temperature data, leading to false fever sensations.
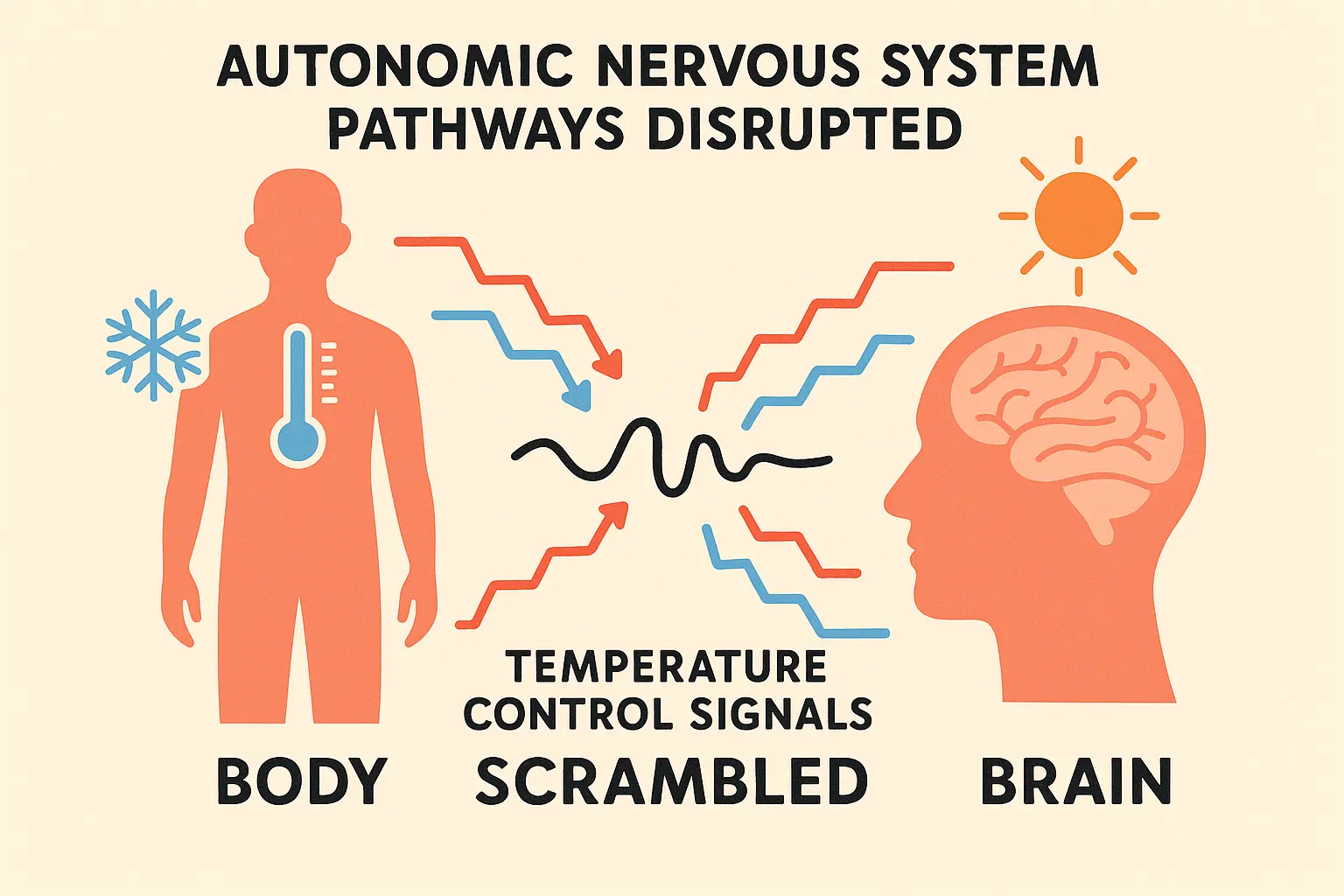
Your Automatic Temperature Responses Go Haywire
Dehydration impairs your autonomic nervous system, leading to completely inappropriate temperature responses. You might find yourself shivering in a warm room or feeling feverish when it’s actually cool—your body’s automatic temperature controls are essentially malfunctioning.
This nervous system dysfunction can stick around for hours after you start rehydrating, because nervous system recovery takes longer than simple fluid replacement. Proper hydration supports normal function, but recovery from dehydration-induced nervous system problems requires patience and consistent hydration maintenance.
What Actually Works to Feel Better Fast
Recovering from dehydration-induced fever isn’t as simple as chugging a bunch of water. You need a systematic approach that addresses electrolyte balance, getting water into your cells, and timing. I’ve learned there’s actually a specific sequence that works best for getting your temperature regulation back on track.
Adults with internal Adults with internal body temperatures between 100.4 and 102.2 degrees Fahrenheit have a low-grade fever, and while these aren’t usually life-threatening, they can be warning signs of severe dehydration requiring immediate medical attention.
The recovery process involves multiple phases, each targeting different aspects of the temperature dysfunction. People who follow this structured approach recover faster and more completely than those who just drink water randomly throughout the day.
Understanding the science behind effective rehydration has completely changed how I approach temperature-related symptoms. The dehydration headache, fatigue, and fever-like sensations all respond to specific interventions when applied in the right sequence.
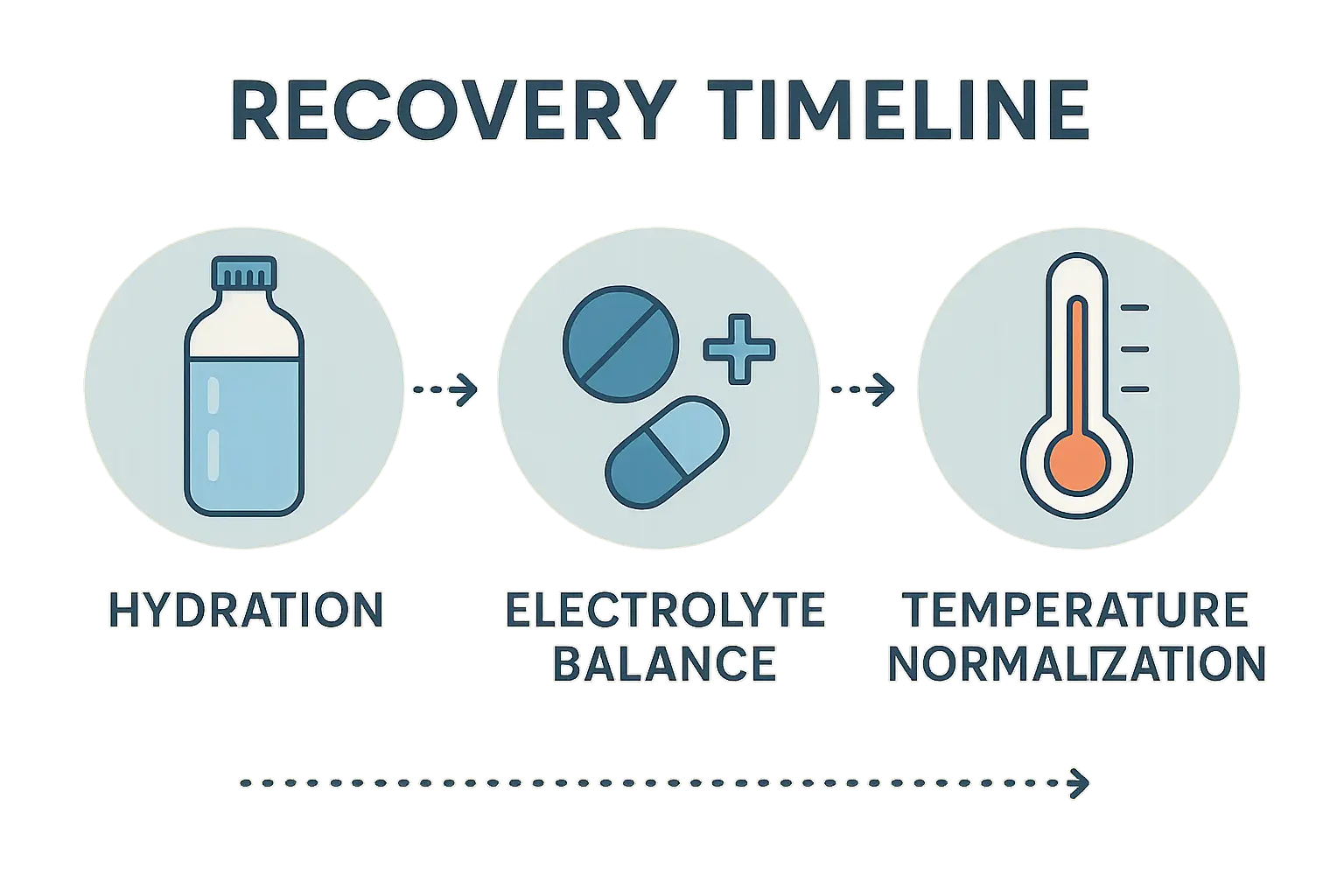
The Rehydration Strategy That Actually Works
Effective recovery requires specific fluid replacement strategies that go way beyond just drinking water. You need to optimize electrolyte balance, timing, and cellular uptake to actually reverse the temperature problems that dehydration causes.
Most people make critical mistakes during rehydration that can actually make their symptoms last longer or create new problems. Drinking too much plain water too quickly can dilute your remaining electrolytes, making things worse rather than better.
The thing is, dehydration affects multiple body systems at once, so recovery has to address cellular function, blood volume, electrolyte balance, and nervous system function all together. When you’re properly hydrated, all these systems work seamlessly.
Proper rehydration often requires more than just water, and understanding how dehydration affects nausea and other symptoms helps you recognize when professional intervention may be necessary. Severe cases may require medical supervision to prevent complications during recovery.
The Right Order for Electrolytes
There’s an optimal rehydration sequence that most people get wrong. You need sodium first to restore blood volume, then potassium for cellular function, followed by magnesium for metabolic recovery. Here’s what actually works:
- Start with 16-20 oz of water mixed with 1/4 teaspoon sea salt within the first hour
- Follow with 8 oz of water every 30 minutes for the next 2-3 hours
- Add magnesium and potassium after your initial sodium replacement
- Watch your urine color go from dark yellow to pale yellow
This sequence addresses your body’s priorities during recovery. Sodium comes first because your cardiovascular system needs adequate blood volume to function. Without proper blood volume, your cells can’t receive the nutrients they need for recovery.
The timing matters because flooding your system with electrolytes all at once can overwhelm your kidneys and create additional stress. Gradual replacement allows your body to use each mineral effectively while maintaining proper balance throughout recovery.
| Recovery Phase | Time Frame | Fluid Type | Electrolyte Focus | Expected Temperature Response |
|---|---|---|---|---|
| Emergency Phase | 0-1 hour | Water + sea salt | Sodium restoration | Temperature may continue rising |
| Stabilization Phase | 1-3 hours | Water every 30 min | Balanced electrolytes | Temperature plateau |
| Cellular Recovery | 3-6 hours | Water + minerals | Potassium & magnesium | Temperature begins normalizing |
| Full Recovery | 6-24 hours | Maintenance hydration | Complete mineral balance | Temperature fully normalized |
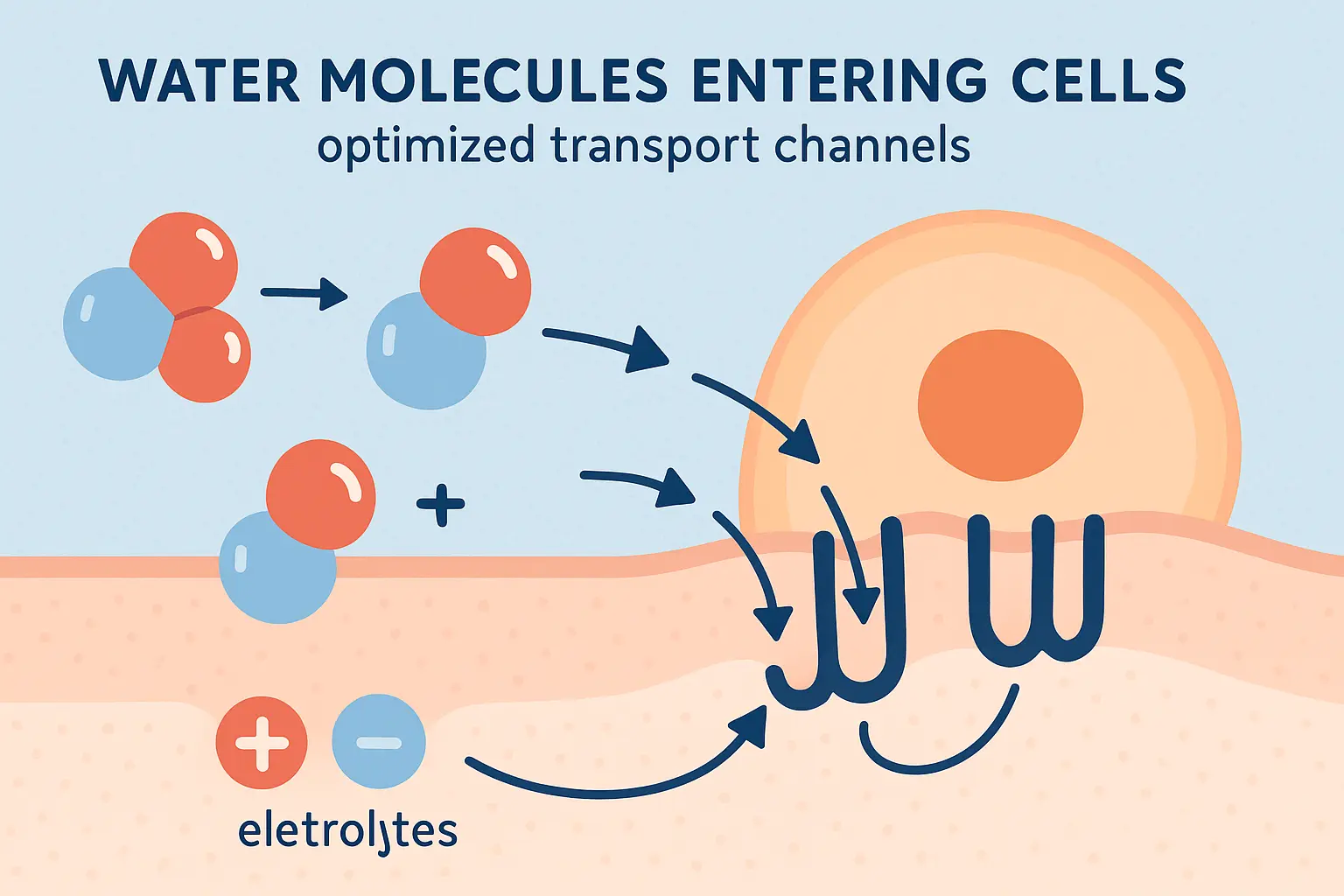
Getting Water Into Your Cells (Not Just Your Stomach)
True cellular rehydration requires specific nutrients and timing to ensure water reaches your dehydrated cells instead of just passing through your system. Here’s how to optimize cellular uptake:
- Drink water at room temperature (cold water can shock dehydrated systems)
- Add a pinch of high-quality sea salt to every 16 oz of water
- Include a little glucose or natural fruit juice to activate cellular transporters
- Space consumption over 4-6 hours rather than chugging large amounts quickly
Your cells have specific transporters that pull water inside when sodium and glucose are present together. Without this combination, water can pass through your digestive system without actually reaching the cells that need it most.
Temperature matters because your digestive system works more efficiently when fluids are close to body temperature. Cold fluids require energy to warm up, and when you’re already dealing with dehydration stress, you want to minimize additional energy demands.
Catching Dehydration Before It Catches You
Preventing dehydration-induced fever means understanding your individual risk factors and implementing hydration strategies before symptoms appear. You need to monitor specific signs that reveal early dehydration before your temperature regulation gets thrown off.
Prevention is always more effective than treatment, especially with temperature regulation issues. Once your body’s thermostat gets confused by dehydration, recovery takes significantly longer than simply maintaining proper hydration from the start.
The signs and symptoms of dehydration often appear in a predictable sequence, and recognizing the early warning signs can prevent the more serious temperature-related complications that develop with severe fluid loss.
The Warning Signs That Actually Matter
Advanced hydration monitoring uses specific signs to detect early dehydration before temperature problems occur. Here are the key things to track:
- Monitor first morning urine color (should be pale yellow)
- Check skin tent test on back of hand (should return to normal within 2 seconds)
- Track body weight fluctuations (more than 2% loss indicates significant dehydration)
- Pay attention to cognitive function and mood changes as early warnings
These signs give you objective data about your hydration status before you feel symptoms. By the time you feel thirsty, your body has already been managing fluid deficits for hours.
Morning urine color is particularly valuable because it reflects your overnight hydration status without interference from recent fluid intake. Dark yellow or amber-colored urine indicates concentrated waste products that signal inadequate fluid reserves.
The skin test provides immediate feedback about tissue hydration levels. When you’re properly hydrated, your skin snaps back quickly after being pinched. Delayed return indicates that your tissues are already pulling water from less critical areas to maintain vital functions.
Simple Prevention Checklist:
- ☐ Drink 16-20 oz of water when you wake up
- ☐ Check urine color before your first bathroom break
- ☐ Weigh yourself at the same time daily
- ☐ Do the skin test weekly
- ☐ Pay attention to energy levels and mental clarity
- ☐ Increase fluids before outdoor activities
- ☐ Set hourly hydration reminders during busy days
- ☐ Keep electrolyte supplements handy for recovery

Understanding this complex relationship between dehydration and temperature regulation shows why personalized health monitoring matters so much. When you’re dealing with unexplained fever, fatigue, or brain fog that might stem from chronic dehydration, you need more than just generic advice—you need targeted intervention based on your unique physiology.
Enov.one’s comprehensive telemedicine approach recognizes that these symptoms often indicate deeper metabolic imbalances. Their personalized assessments can identify underlying factors such as nutrient deficiencies (particularly B12 for cellular energy), hormonal imbalances affecting fluid retention, or metabolic inefficiencies that increase your hydration needs. Through tailored supplementation programs and integrated health monitoring, they address root causes rather than just surface symptoms.


Bottom Line
Can dehydration cause a fever? Absolutely, and the reasons why are more complex than most people realize. Your body’s temperature regulation involves cellular energy production, immune responses, nervous system function, and cardiovascular performance—all of which can be disrupted by inadequate hydration.
What strikes me most about this whole topic is how interconnected everything is in your body. Your cells, blood vessels, immune system, and nervous system all work together to maintain normal temperature, and dehydration can disrupt every single one simultaneously. That’s why recovery requires such a strategic approach—you’re helping multiple body systems get back in sync.
The key takeaway? Don’t wait until you feel thirsty or feverish to think about hydration. By the time you notice symptoms, your body’s already been struggling for a while. Pay attention to those early warning signs, follow proper rehydration protocols when needed, and remember that sometimes the simplest explanation can cause the most confusing symptoms.
If you feel feverish but your thermometer says you’re fine, grab some water with a little salt and see how you feel in an hour. Your body might just be telling you it needs more fluids. It’s one of those simple solutions to what feels like a complicated problem.
